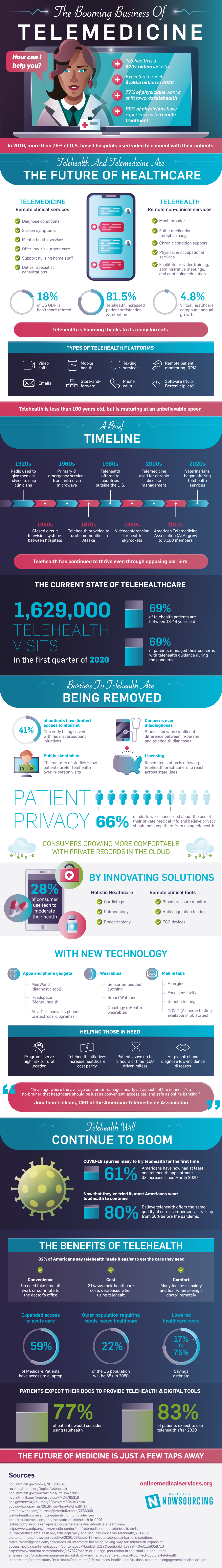
The pandemic, with its need for isolation, gave a major boost to the development of new ways to diagnose or treat, this was the impetus for the development of telemedicine software development services. Online medicine, which was shunned not so long ago, has become ubiquitous and, moreover, in-demand among customers. But still, many are wary of this option of interacting with a doctor. Let’s figure out what it is, how it works, and how telemedicine solutions can impact healthcare institutions and patients.
What is telehealth software?
IT technology in healthcare is not just the use of gadgets and other devices. This is a whole complex of both software and hardware that is used to store, distribute and analyze health data.
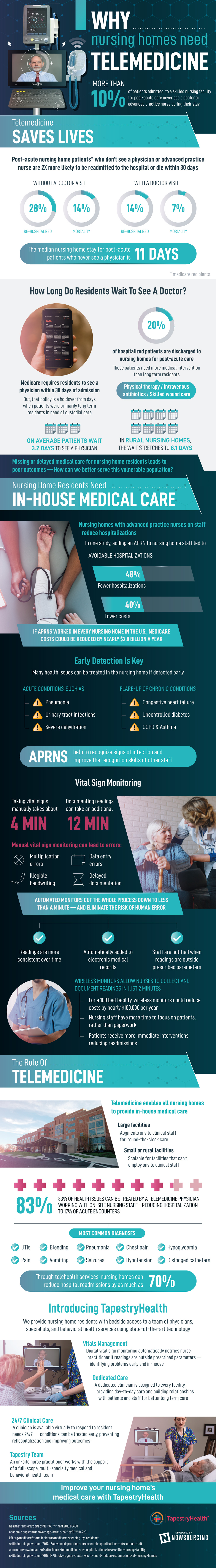
Traditional clinical services, patient monitoring, and record-keeping have now been transformed and simplified with the advent and spread of telemedicine. This also includes remote training of medical personnel. The use of telemedicine software has simplified and popularized video consultations, digital imaging, remote medical diagnosis, and more.
And if we are talking about software for telemedicine, then we must understand what types of it are:
Real-time telemedicine communication software
The software and the scenario of its use are most comparable to a real visit to the doctor. Both the doctor and the patient can discuss issues of interest remotely. This gives doctors the opportunity to assess the patient’s condition and carry out treatment remotely. And for the patient, this option of telemedicine makes it possible to contact a remote specialist or institution for consultation.
Telemedicine platforms for data storage and transfer
This is a step towards transformation in the exchange of information. It is mainly used in the exchange of digital photos and videos for diagnostic purposes, or clinical data between patients and the clinic, or between doctors for additional consultations.
Remote patient monitoring
The target application is home telemedicine. This allows patients to be under constant supervision. It consists of specialized software and equipment that is installed at patients’ homes. This complex also includes monitoring the vital signs of patients and also provides doctors with frequent updates on the well-being of patients.
Integration of telemedicine software
This software is aimed at integration with existing medical systems. These are comprehensive solutions that are aimed at the complete synchronization of all patient credentials and their treatment histories. We can say that this is the way to centralize data.
Integration with Pharmaceuticals
Patients can access many of the professional services given by pharmacies and receive guidance on pharmaceutical therapy management remotely by using telemedicine software.
Benefits of using telemedicine solutions
All of the methods for incorporating software in medicine described above are applicable at all levels of care. Consider some easy instances.
Attempts to get treatment from a doctor in another city or to make suggestions to a patient who lives in another city have always existed. Doctors have sent letters and called patients. However, telemedicine truly took off in the country when the Internet became available in practically every home. It’s a simple and rapid way to communicate, allowing the doctor to provide as much information as possible from a distance.
When a person knows what telemedicine is, he or she can get help in situations where a visit to the doctor is impossible or undesirable. For example:
● The trip to the hospital is long and difficult (the patient has a fever, something hurts a lot, there is a lot of weakness), and the wait for the doctor on duty is long;
● The problem seems non-hazardous or irrelevant, and the person is not ready to spend the whole working day for it, but wants to get confirmation from the doctor that there is nothing to worry about;
● Hospitals are overloaded because of an emergency or natural disaster, so it is impossible to get help there for a minor illness or a chronic problem;
● Because of the quarantine, it is undesirable to go out and even more so to communicate with doctors through whom many sick people pass;
● The illness suddenly appeared suddenly while on a business trip or during a trip to another country where there is no possibility to get qualified help or there is no possibility to invite an experienced interpreter who could explain all the details;
By contacting a doctor online, a person avoids having to sit in lines, spend time on travel and money on time off work in order to get to an appointment on time.
Custom development of telemedicine software
When it comes to developing software for the telemedicine industry, the benefits provided by specialized and even custom applications include:
● More convenient and cheap patient care: real-time consultations, photo-based consultations, including staging solutions, and mobile healthcare accessible.
● Telemedicine solutions help make processes more economical, but at the same time more efficient. Thanks to comprehensive solutions, it is much easier for the patient to see a doctor online, and because of this, transport costs and non-urgent visits to clinics are reduced.
● The storage of medical data is also undergoing changes. Telemedicine solutions allow you to handle huge amounts of data with complete security and precise control.
● Brings automation to medical processes. This aspect has a positive effect on the time spent by doctors and on administrative operations.
But also, custom software may provide some problems too. We at Empeek regularly face the following challenges associated with developing telemedicine applications:
● Licensing and compliance with laws make development difficult.
● Difficulties in building a connection with the server part, since all information exchange must be centralized.
● The provision of platforms should be at the highest level. Telemedicine involves a lot of personal data of users, their medical history and other information that needs to be protected. And besides, you still need to ensure the security of payments.
● Creation of high-quality UI / UX to provide a single space for all parties of communication.
The value of telemedicine software development services is to provide you with a solution based on in-depth market analysis and tailored to your individual needs.